Tibialis Posterior Tendinopathy
- Tibialis Posterior Tendinopathy
Tibialis Posterior Tendinopathy
What is a Tibialis Posterior Tendinopathy?
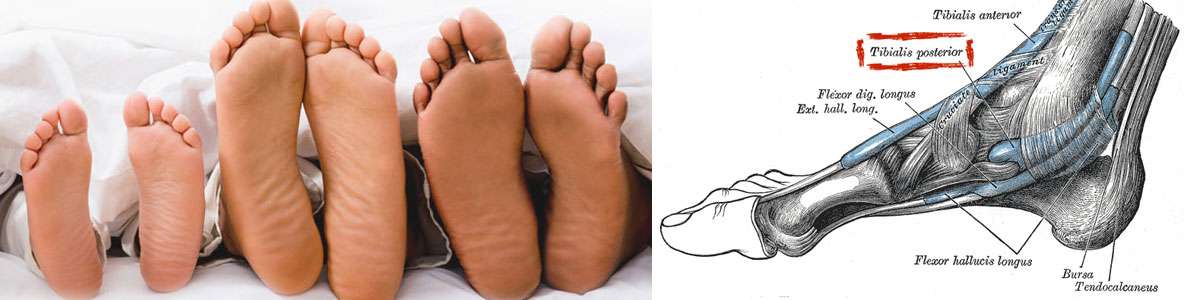
The tibialis posterior muscle has a tendon that runs down the inside of your lower leg and behind your ankle bone (medial malleolus) and joins on to your midfoot. Its job is to help support our foot arch and to support your ankle.
What are Tendons?
Tendons are the tough fibres that connect muscle to bone. Most tendon injuries occur near joints, such as the shoulder, elbow, knee, and ankle. A tendon injury may seem to happen suddenly, but usually, it is the result of many tiny tears to the tendon that have happened over time. Health professionals may use different terms to describe a tendon injury. You may hear:
Tendinitis (or Tendonitis): This actually means “inflammation of the tendon,” but inflammation is rarely the cause of tendon pain.
Tendinosis: This refers to tiny tears in the tissue in and around the tendon caused by overuse.
Tendinopathy: This is an umbrella term that can refer to either tendinitis or tendinosis. As it is common to find areas of both tendinosis and tendinitis in the same tendon, the term tendinopathy is often used.
Tibialis Posterior injuries can include:
- Tibialis Posterior tendinitis (an inflamed tendon).
- Tibialis Posterior tendinosis (a non-inflamed degenerative tendon).
- Tibialis Posterior tenosynovitis (an inflamed tendon sheath).
- a ruptured Tibialis Posterior tendon (secondary to degeneration or tear).
What Causes Tibialis Posterior Tendinopathy?
Tibialis Posterior Tendinitis or Tendinosis is nearly always caused by an overloading of the tendon especially where it curves around your ankle bone. The overloading of the tendon can be due to excessive weight, as in loaded calf raises, overtraining such as through a significant increase in running time or intensity, or a combination of the two such as an increase in jumping exercise or activities.
Common Causes of Tibialis Posterior Tendinopathy include:
- Over-training or unaccustomed use too much too soon
- A period of under-training, then moving back to previous training loads
- A sudden change in training surface e.g. grass to bitumen
- Flat (over-pronated) feet
- Tight hamstring (back of thigh) and calf muscles
- Toe walking (or constantly wearing high heels)
- Poorly supportive footwear, or a change in footwear (even to new shoes!)
- Hill running
- Poor eccentric strength
How is Tibialis Posterior Tendinopathy Diagnosed?
Your physiotherapist or sports doctor can usually confirm the diagnosis of Tibialis Posterior tendinopathy in the clinic. They will base their diagnosis on your history, symptom behaviour and clinical tests.
What are the Aims of Tibialis Posterior Tendinopathy Treatment?
Tibialis Posterior tendinopathy is a relatively common problem that we see at PhysioWorks and it is, unfortunately, an injury that often recurs if you return to sport too quickly especially if a thorough rehabilitation program is not completed.
What is the Treatment for Tibialis Posterior Tendinopathy?
As with most soft tissue injuries the initial treatment is RICE – Rest, Ice, Compression and Elevation.
In the early phase you’ll be unable to walk without a limp, so your Tibialis Posterior tendon needs some active rest from weight-bearing loads. You may need to be non or partial-weight-bearing, utilise crutches, a wedged Achilles walking boot or heel wedges to temporarily relieve some of the pressure on the Tibialis Posterior tendon. Your physiotherapist will advise you on what they feel is best for you.
Ice is a simple and effective modality to reduce your pain and swelling. Please apply for 20-30 minutes each 2 to 4 hours during the initial phase or when you notice that your injury is warm or hot. Anti-inflammatory medication (if tolerated) and natural substances eg arnica may help reduce your pain and swelling. However, it is best to avoid anti-inflammatory drugs during the initial 48 to 72 hours when they may encourage additional bleeding. Most people can tolerate paracetamol as a pain reducing medication.
Phase 2: Regain Full Range of Motion
If you protect your injured Tibialis Posterior tendon appropriately the torn tendon fibres will successfully reattach. Mature scar formation takes at least six weeks. During this time period, you should be aiming to optimally remold your scar tissue to prevent a poorly formed scar that will re-tear in the future.
Phase 3: Restore Eccentric Muscle Strength
Phase 4: Restore Concentric Muscle Strength
Phase 5: Normalise Foot Biomechanics
Tibialis Posterior tendon injuries can occur from poor foot biomechanics eg flat foot.
In order to prevent a recurrence, your foot will be assessed. In some instances, you may require a foot orthotic (shoe insert) or you may be a candidate for the Active Foot Posture Stabilisation program.
Phase 6: Restore High Speed, Power, Proprioception & Agility
Most Tibialis Posterior tendon injuries occur during high-speed activities, which place enormous forces on your body (contractile and non-contractile). In order to prevent a recurrence as you return to sport, your physiotherapist will guide you with exercises to address these important components of rehabilitation to both prevent a recurrence and improve your sporting performance.
Phase 7: Return to Sport
Depending on the demands of your chosen sport, you will require specific sport-specific exercises and a progressed training regime to enable a safe and injury-free return to your chosen sport.